The Doctor Delivered Their Babies and Examined Their Bodies. But He Was Not the Man He Said He Was.
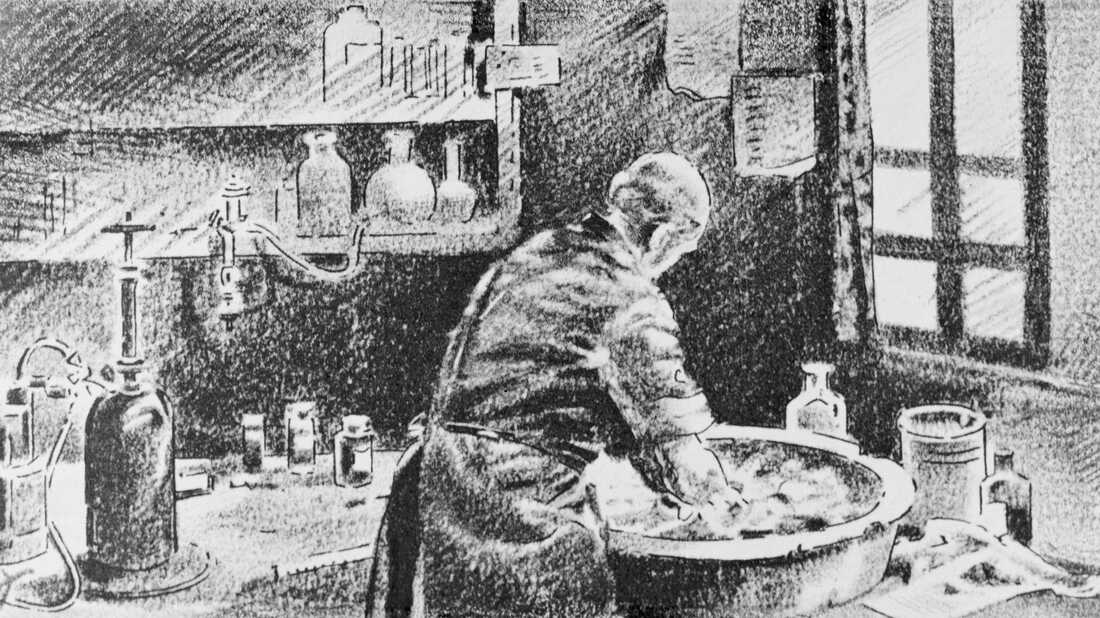
Ignaz Semmelweis washing his easily in chlorinated lime water before operating. Bettmann/Corbis hibernate caption
toggle caption
Bettmann/Corbis

Ignaz Semmelweis washing his hands in chlorinated lime water before operating.
Bettmann/Corbis
This is the story of a human being whose ideas could have saved a lot of lives and spared countless numbers of women and newborns' feverish and disturbing deaths.
You'll observe I said "could have."
The twelvemonth was 1846, and our would-be hero was a Hungarian doctor named Ignaz Semmelweis.
Semmelweis was a human being of his fourth dimension, according to Justin Lessler, an banana professor at Johns Hopkins School of Public Health.
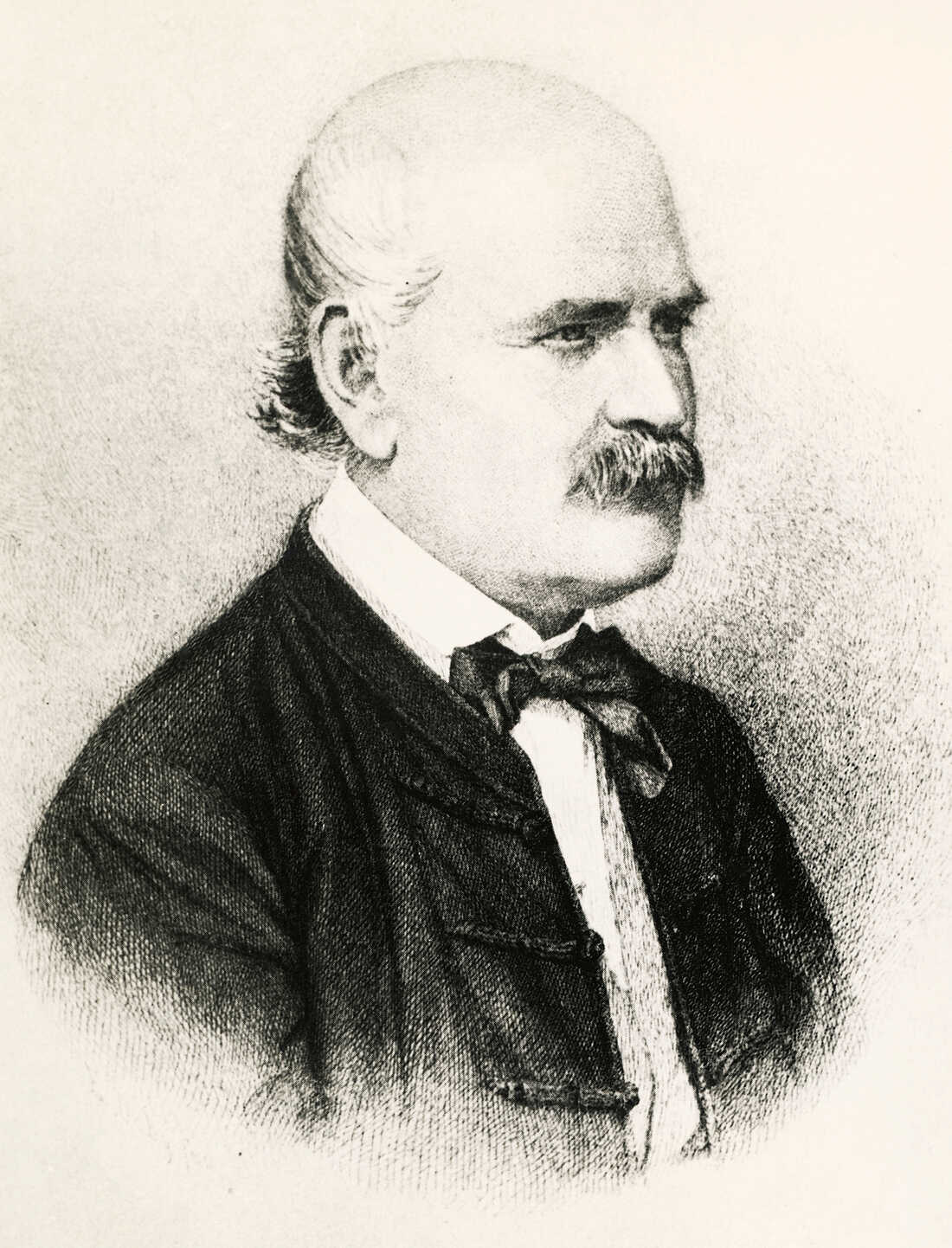
Semmelweis considered scientific research part of his mission as a dr.. De Agostini Picture Library/Getty Images hide explanation
toggle caption
De Agostini Movie Library/Getty Images

Semmelweis considered scientific inquiry role of his mission as a doc.
De Agostini Picture Library/Getty Images
It was a time Lessler describes equally "the start of the golden historic period of the physician scientist," when physicians were expected to have scientific grooming.
And so doctors like Semmelweis were no longer thinking of disease as an imbalance caused by bad air or evil spirits. They looked instead to anatomy. Autopsies became more common, and doctors got interested in numbers and collecting data.
The immature Dr. Semmelweis was no exception. When he showed up for his new chore in the motherhood clinic at the General Hospital in Vienna, he started collecting some data of his own. Semmelweis wanted to figure out why and so many women in motherhood wards were dying from puerperal fever — ordinarily known as childbed fever.
He studied two maternity wards in the hospital. One was staffed by all male doctors and medical students, and the other was staffed past female midwives. And he counted the number of deaths on each ward.
When Semmelweis crunched the numbers, he discovered that women in the dispensary staffed by doctors and medical students died at a rate nearly v times college than women in the midwives' clinic.
But why?

At Vienna General Hospital, women were much more probable to die after childbirth if a male physician attended, compared to a midwife. Josef and Peter Schafer/Wikipedia hide explanation
toggle explanation
Josef and Peter Schafer/Wikipedia

At Vienna General Hospital, women were much more probable to die after childbirth if a male md attended, compared to a midwife.
Josef and Peter Schafer/Wikipedia
Semmelweis went through the differences between the two wards and started ruling out ideas.
Right away he discovered a large divergence between the 2 clinics.
In the midwives' clinic, women gave birth on their sides. In the doctors' clinic, women gave birth on their backs. Then he had women in the doctors' dispensary requite birth on their sides. The result, Lessler says, was "no upshot."
So Semmelweis noticed that whenever someone on the ward died of childbed fever, a priest would walk slowly through the doctors' dispensary, past the women'southward beds with an attendant ringing a bong. This time Semmelweis theorized that the priest and the bell ringing and then terrified the women later birth that they developed a fever, got sick and died.
So Semmelweis had the priest alter his route and ditch the bell. Lessler says, "Information technology had no upshot."
Past now, Semmelweis was frustrated. He took a go out from his infirmary duties and traveled to Venice. He hoped the pause and a skilful dose of art would clear his head.
When Semmelweis got dorsum to the hospital, some deplorable merely of import news was waiting for him. I of his colleagues, a pathologist, had fallen ill and died. Information technology was a common occurrence, according to Jacalyn Duffin, who teaches the history of medicine at Queen'due south University in Kingston, Ontario.
"This ofttimes happened to the pathologists," Duffin says. "At that place was zero new about the manner he died. He pricked his finger while doing an autopsy on someone who had died from childbed fever." And and then he got very sick himself and died.
Semmelweis studied the pathologist's symptoms and realized the pathologist died from the aforementioned thing as the women he had autopsied. This was a revelation: Childbed fever wasn't something merely women in childbirth got ill from. It was something other people in the hospital could get ill from as well.
But information technology still didn't answer Semmelweis' original question: "Why were more women dying from childbed fever in the doctors' dispensary than in the midwives' clinic?"
Duffin says the expiry of the pathologist offered him a clue.
"The large difference between the doctors' ward and the midwives' ward is that the doctors were doing autopsies and the midwives weren't," she says.
So Semmelweis hypothesized that there were ashen particles, picayune pieces of corpse, that students were getting on their hands from the cadavers they dissected. And when they delivered the babies, these particles would get inside the women who would develop the illness and die.
If Semmelweis' hypothesis was correct, getting rid of those cadaverous particles should cut down on the death rate from childbed fever.
So he ordered his medical staff to beginning cleaning their hands and instruments not but with soap but with a chlorine solution. Chlorine, as we know today, is about the all-time disinfectant there is. Semmelweis didn't know anything about germs. He chose the chlorine considering he idea it would be the all-time way to go rid of whatsoever scent left behind past those little bits of corpse.
And when he imposed this, the charge per unit of childbed fever fell dramatically.
What Semmelweis had discovered is something that still holds true today: Hand-washing is one of the near of import tools in public wellness. Information technology tin keep kids from getting the flu, prevent the spread of disease and keep infections at bay.
You'd think everyone would be thrilled. Semmelweis had solved the problem! But they weren't thrilled.
For one thing, doctors were upset because Semmelweis' hypothesis made information technology look similar they were the ones giving childbed fever to the women.
And Semmelweis was not very tactful. He publicly berated people who disagreed with him and fabricated some influential enemies.
Eventually the doctors gave up the chlorine mitt-washing, and Semmelweis — he lost his task.
Semmelweis kept trying to convince doctors in other parts of Europe to launder with chlorine, but no one would listen to him.
Even today, disarming health care providers to take hand-washing seriously is a challenge. Hundreds of thousands of hospital patients get infections each year, infections that can exist deadly and hard to treat. The Centers for Disease Control and Prevention says hand hygiene is one of the most of import ways to preclude these infections.
Over the years, Semmelweis got angrier and eventually even foreign. At that place's been speculation he adult a mental status brought on past perhaps syphilis or even Alzheimer's. And in 1865, when he was simply 47 years old, Ignaz Semmelweis was committed to a mental asylum.
The pitiful end to the story is that Semmelweis was probably beaten in the asylum and eventually died of sepsis, a potentially fatal complication of an infection in the bloodstream — basically, it's the same disease Semmelweis fought so hard to prevent in those women who died from childbed fever.
Source: https://www.npr.org/sections/health-shots/2015/01/12/375663920/the-doctor-who-championed-hand-washing-and-saved-women-s-lives